QuickLift™:Separating Fact From Fiction In Less Invasive Facelift Surgery(2)
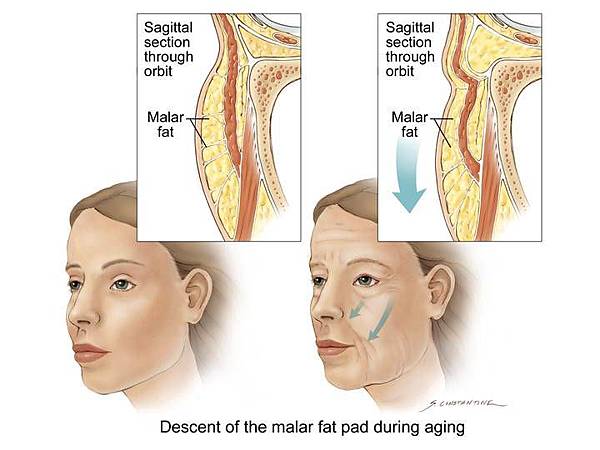
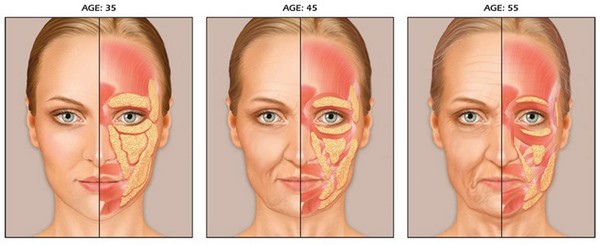
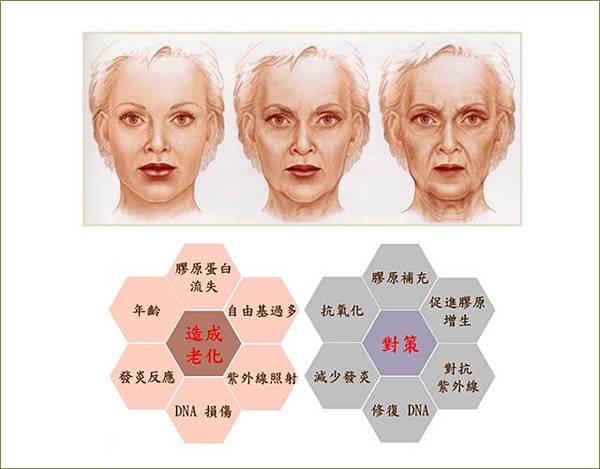
We joke that gravity catches up with us. Like many jokes, there is truth in this one. As we age, we begin to sag at the jowls and around the eyes. The face we present to the world reflects less and less how we feel on the inside, the older we become.
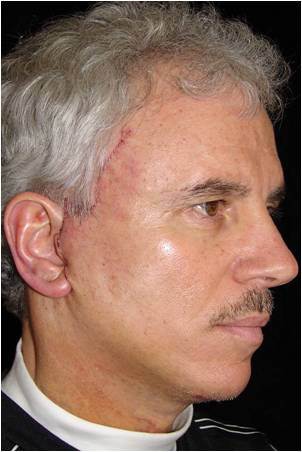
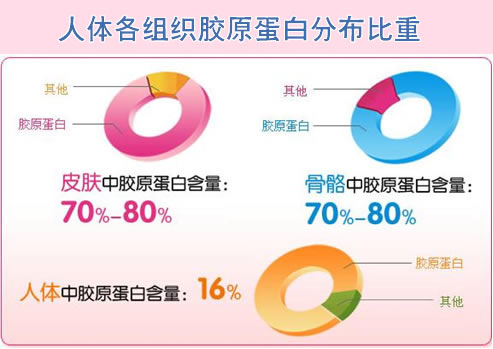
This visible process of aging is more pronounced for women, who typically have thinner skin than men. It is not an old wife’s tale that women appear to age more quickly than men. It is scientific fact. In the first five years of menopause, for example, women’s skin accelerates from 1 percent annual loss in tonal quality to 6 percent a year, or 30 percent loss in those five years alone. After the first five years of menopause, the rate of decrease continues at 2.1 percent a year for women. While the changes for women may be more dramatic at first, the same aging process catches up with men, which is why 15-20 percent of all facelift patients today are men.
Thanks to modern cosmetic surgery, this rapid and sometimes startling change in the face we present to the world does not have to define who we are. We can make surgical and post-surgical changes in how we care for our face that can help us look as young as we feel on the inside. We can make changes in our appearance that spur us to make changes in our lives that lead to better health.
I have seen this time and again with my own patients — cosmetic surgery becomes the “signal point” or second chance in their lives to exercise regularly, lose weight, deal with stress, change jobs, and generally, take better care of themselves. Changing body image through cosmetic surgery can have profound impacts on how patients feel on the inside, improving mental and emotional health as well as physical appearance. Patients report that cosmetic surgery can make you feel better on the inside.
What’s the best type of surgery to present my “real” face to the world?
The cosmetic surgery choice that is best for you will emerge only after you thoroughly investigate potential procedures, doctors, and outcomes. I advise my patients to make the decision that feels and looks right for them. I recommend that you listen to what others have to say. But listen most importantly to your own heart.
After nearly three decades of practice as a cosmetic surgeon, I speak from experience. That experience led me to develop the QuickLift™ and to continually work to perfect the procedure. I work with hundreds of patients each year who are good candidates for the surgery.
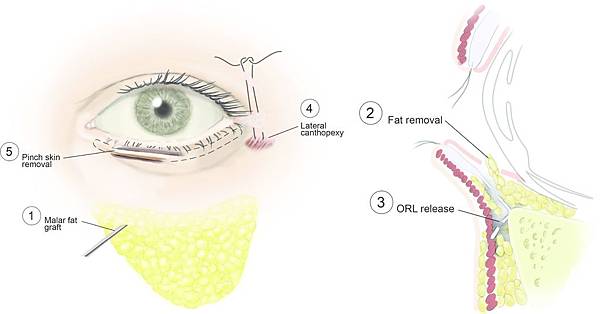
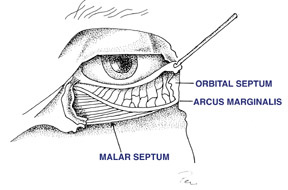
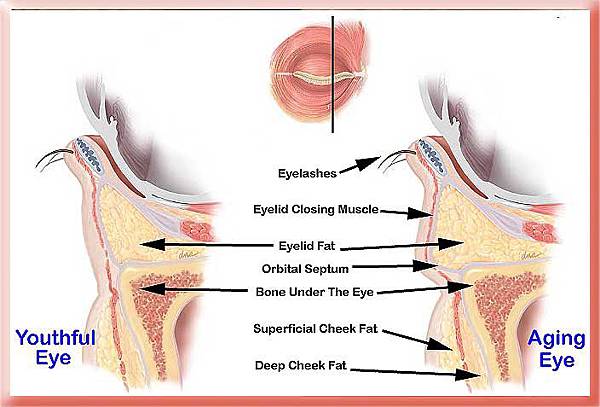
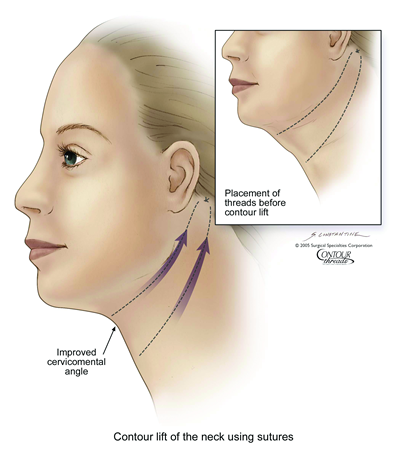
Early facelift procedures were limited in the extent of skin lifting to improve skin tone, and did not address the superficial musculoaponeurotic system (the SMAS, which is the covering of the facial muscles that I work with in performing the QuickLift). Consequently, the medical literature shows these early facelifts had a short life span, sometimes just a few years.
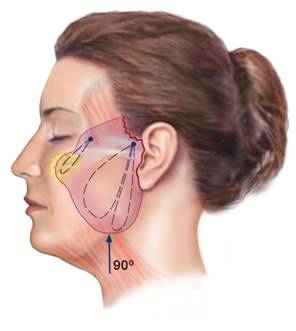
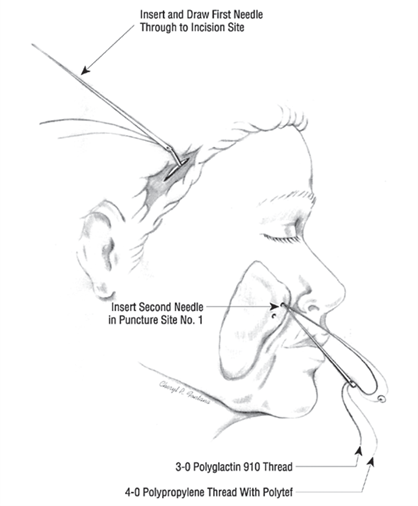
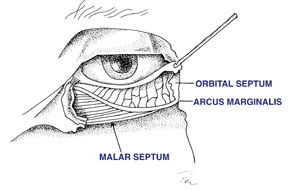
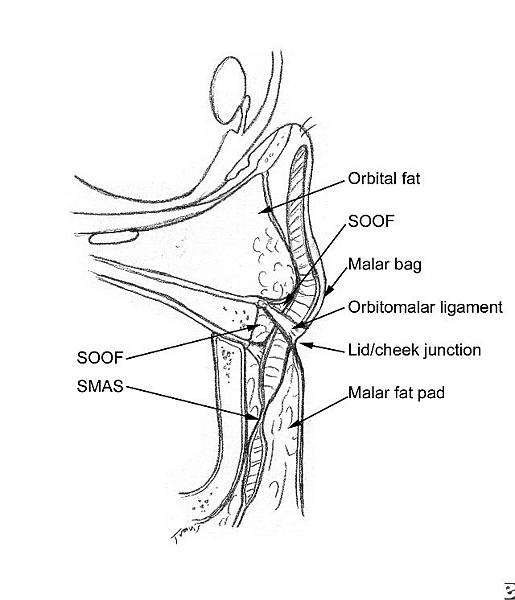
A Visual Comparison of Facelift Procedures
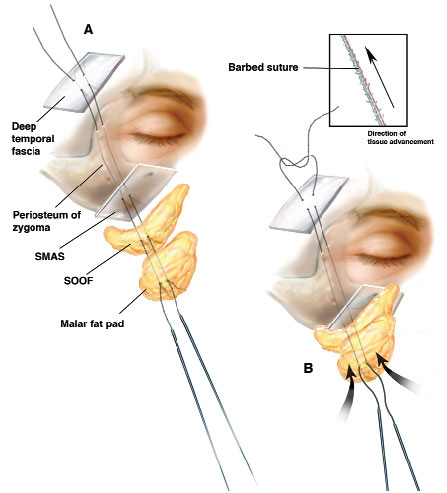
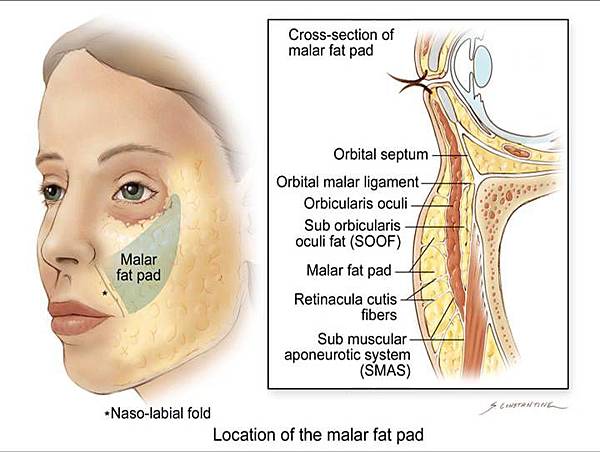
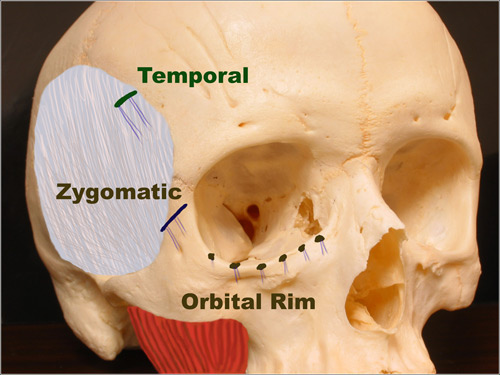
In the early 1990s, the composite rhytidectomy was introduced. This facelift procedure involves aggressive undermining of the face in a deep plane, and the elevations of the SMAS, cheek fat, and the muscles that close the eyelids (orbicularis oculi). Because of its more aggressive nature, this procedure typically has a higher complication rate, and patients can have a relatively long disfigurement period, with four to six weeks off of work and a period of six to 12 months before optimal results are achieved. What I have learned in three decades of practice is that patients with busy lives do not want to deal with prolonged swelling or a higher risk of complications. So when I think of “quick” with regard to the QuickLift™, certain aspects of the surgery come to mind. The most appealing aspect of this procedure is that it typically requires less downtime, meaning a patient can go back to their regular life more quickly. This begins with the surgery itself. It typically takes much less time to perform a QuickLift™ as compared to more extensive facelift surgery. Patients often experience procedure times of 90 minutes and sometimes less; more if adjunctive procedures are added. Second, because of the way the QuickLift™ is performed, patients typically need only local anesthesia, though additional sedative is sometimes indicated and offered by different surgeons. The potential risks, side effects, etc., all grow with more complex surgical procedures that require general anesthesia. And the medical literature shows that, the older we are, the more risk we face with general anesthesia. Third, the QuickLift™ procedure itself is less invasive medically. Traditional “deep plane” facelift surgery for instance, works at a deep skin level where your nerves lie. While this procedure may be best for some patients, the risk of nerve damage cannot be ignored. To work around the nerves, deep plane procedures require more surgical time, and more time in surgery typically calls for more intense anesthesia needs. The QuickLift™, in contrast, is performed in the SMAS layer where there is little chance of nerve damage. In fact, of the thousands of QuickLift™ procedures performed nationally, I am unaware of any cases of permanent nerve damage. Put these important considerations together and it’s clear that if a particular kind of surgery takes less time to do, involves less aggressive anesthesia and less complicated surgical techniques, it is “quicker.” Less time in surgery, with a reduced need for anesthesia and less invasive techniques leads, generally speaking, too much quicker healing and results that are visible much sooner. This is an observable fact based upon thousands of successful procedures that have been documented in the medical literature.
No pain no gain
Even though the inference taken from Quick may be that the QuickLift™ is a drive-through procedure, it is vitally important to understand that the decision to have any surgical procedure, certainly a cosmetic one, is a big one. It is one that, regardless of the selected procedure and the quality of the care, may not lead to the expected outcome. In my title for this section, I did not mean to suggest that facial procedures are painful. By and large, they are not. However, the more aggressive the procedure, the more probable is the increase in the level of discomfort. Conversely, less aggressive typically translates into less discomfort. My point is that there are numerous issues that individuals go through in deciding to pursue facial enhancement. Do they really want a facelift? What type of facelift is best for them? And what doctor do they choose to perform the surgery?
Figure. QuickLiftTM With Minimal Swelling and Bruising Post-Operatively
 QuickLift™ Pre Procedure
QuickLift™ Pre Procedure
 QuickLift™ 3 Days Post Procedure
QuickLift™ 3 Days Post Procedure
 QuickLift™ 7 Days Post Procedure
QuickLift™ 7 Days Post Procedure
Without going into great detail, here are some of the possible “curveballs” that may lead to a longer, or possibly, impeded journey to an expected outcome:
EXPECTATION:regardless of how well a doctor performs a facelift or QuickLift™, if the patient is expecting yin, and they get a yang, there will be some discontent. That is where consultation comes into play. Consultation is the ideal forum to create a realistic plan with the doctor in a private setting. What can reasonably be expected from the procedure relative to the facial conditions and goals of YOU, the patient?No procedure including the QuickLift™ is a cookie-cutter procedure. It must be customized to meet the various nuances that make each of our faces unique. This starts and often ends with the consultation.







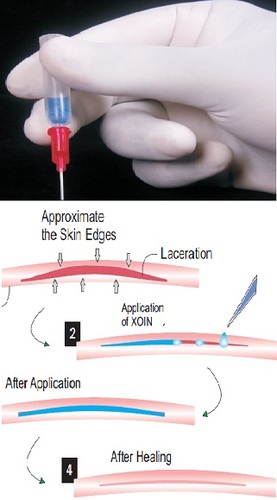

 Discoloration days post-procedure.
Discoloration days post-procedure. Patient same day with hair camouflaging area.
Patient same day with hair camouflaging area.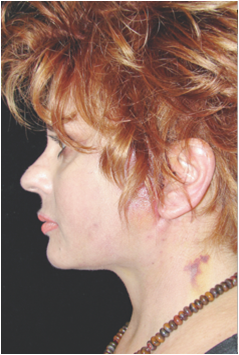 QuickLift™
QuickLift™
 QuickLift™ Pre Procedure
QuickLift™ Pre Procedure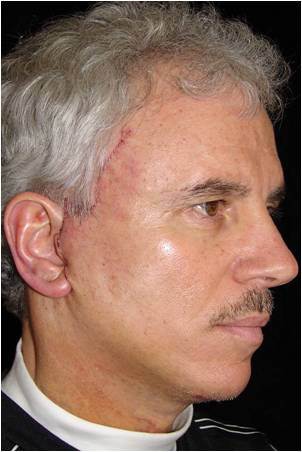 QuickLift™ 3 Days Post Procedure
QuickLift™ 3 Days Post Procedure QuickLift™ 7 Days Post Procedure
QuickLift™ 7 Days Post Procedure
 Fig. 4a (before)
Fig. 4a (before)  Fig. 4b (after)
Fig. 4b (after)  Fig. 5a (before)
Fig. 5a (before)  Fig. 5b (after)
Fig. 5b (after)  Fig. 6a (before)
Fig. 6a (before)