Regeneration of human bones in hip Osteonecrosis and human cartilage in knee Osteoarthritis with autologous Adipose-tissue-derived stem cells:a case series(3)
The third case concerns a 70-year-old Korean woman with over five years' history of right knee pain due to osteoarthritis.
Due to her occupation, she made active use of her bilateral knee joints. With a diagnosis of osteoarthritis of the right knee, she had received multiple injections of steroids and hyaluronic acid over the years. However, she did not notice any improvement in her pain. She was seen by an orthopedic surgeon and was offered a total knee replacement (TKR). She was reluctant to go through the TKR procedure due to possible side effects. Since then, she has been receiving physical therapy with little improvement.
At the time of initial evaluation, she reported moderately severe pain (VAS score 7) on rest. Her knee pain increased when walking. She also complained of mild knee swelling. On physical examination, there was mild joint swelling, a decreased range of motion and tenderness with flexion. Apley and McMurray tests were negative, and there was no ligament laxity.
A pre-treatment 1.5T MRI scan demonstrated a decreased size and deformed contour on the medial meniscus of the left knee due to maceration.
After obtaining ADSCs and preparing PRP as described above for the first two patients, she was prepared for injection of the mixture into the joint.
In order to inject the stem cell and PRP mixture, she was first placed in a supine position with her right knee bent at 90°. After cleaning with povodine-iodine and draping with sterile drapes, her knee was anesthetized with 2% Lidocaine at the medial and lateral sides of the inferior patella. Using a 22-gauge 1-inch needle, 8.5 cm3 of ADSCs, PRP, Dexamethasone and Hyaluronic acid mixture was injected into the medial and the lateral sides of the knee.
She was then instructed to remain still for 30 minutes to allow for cell attachment. As she was subsequently discharged from the clinic, she was instructed to maintain activity as tolerable.
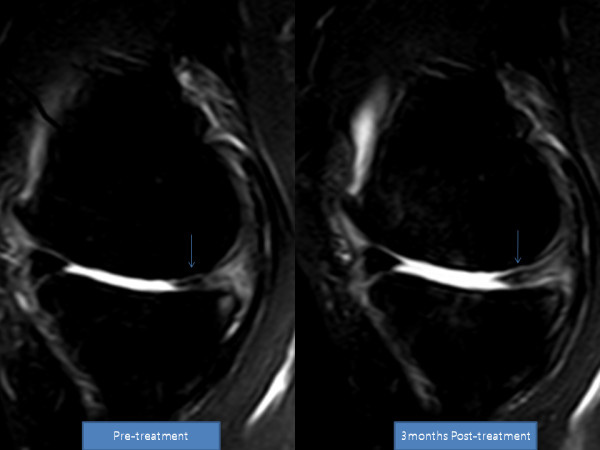
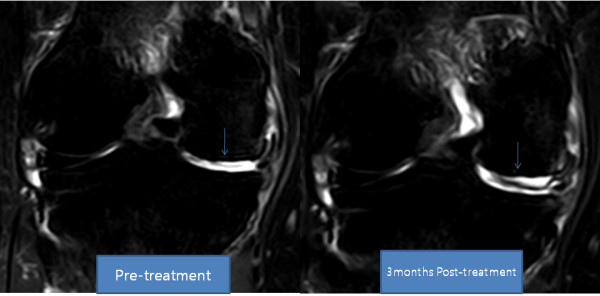
She returned to our clinic for Four additional PRP and Dexamethasone injections over the next four weeks. After the seventh week of ADSC injection, her pain had improved more than 80% and flexion of the knee had also improved. By week 12, her pain had improved more than 90% and the range of motion also further improved (Tables 5 and 6). A post-treatment MRI taken at week 12 showed a significant increase in the thickness of meniscus cartilage on the medial side of the right knee (Figures 3 and 4).
Table 5. Functional rating index and visual analog scale (VAS) score of patient 3
Table 6. Physical therapy (PT), range of motion of patient 3
Figure 3. MRI sagittal T2 view of the knee. Pre-treatment and post-treatment MRI shows increased height of medial meniscus cartilage and articular cartilage (arrow).
Figure 4. MRI coronal T2 view of the knee. Pre-treatment and post-treatment MRI shows increased height of medial meniscus (arrow).



 留言列表
留言列表
