Regeneration of human bones in hip Osteonecrosis and human cartilage in knee Osteoarthritis with autologous Adipose-tissue-derived stem cells:a case series(1)
Jaewoo Pak
Correspondence:Jaewoo Pak jaewoopak@paksmedical.com
Author Affiliations
Miplant Stems Clinic, 32-3 Chungdam-Dong, Gangnam-Gu, Fourth Floor, Seoul, Korea
Journal of Medical Case Reports 2011, 5:296
doi:10.1186/1752-1947-5-296
The electronic version of this article is the complete one and can be found online at:http://www.jmedicalcasereports.com/content/5/1/296
Received:11 October 2010
Accepted:7 July 2011
Published:7 July 2011
© 2011 Pak; licensee BioMed Central Ltd.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Introduction
This is a series of clinical case reports demonstrating that a Combination of Percutaneously injected autologous Adipose-tissue-derived stem cells, Hyaluronic acid, Platelet rich plasma and Calcium chloride may be able to regenerate Bones in human Osteonecrosis, and with addition of a very low dose of Dexamethasone, Cartilage in human knee Osteoarthritis.
Case reports
Stem cells were obtained from adipose tissue of abdominal origin by digesting lipoaspirate tissue with collagenase. These Stem cells, along with Hyaluronic acid, Platelet rich plasma and Calcium chloride, were injected into the right hip of a 29-year-old Korean woman and a 47-year-old Korean man. They both had a history of right hip osteonecrosis of the femoral head. For cartilage regeneration, a 70-year-old Korean woman and a 79-year-old Korean woman, both with a long history of knee pain due to osteoarthritis, were injected with Stem cells along with Hyaluronic acid, Platelet rich plasma, Calcium chloride and a nanogram dose of Dexamethasone. Pre-treatment and post-treatment MRI scans, physical therapy, and pain score data were then analyzed.
Conclusions
The MRI data for all the patients in this series showed significant positive changes. Probable bone formation was clear in the patients with osteonecrosis, and cartilage regeneration in the patients with osteoarthritis. Along with MRI evidence, the measured physical therapy outcomes, subjective pain, and functional status all improved. Autologous Mesenchymal stem cell injection, in conjunction with Hyaluronic acid, Platelet rich plasma and Calcium chloride, is a promising minimally invasive therapy for Osteonecrosis of femoral head and, with Low-dose Dexamethasone, for Osteoarthritis of human knees.
Background
Adipose-tissue-derived stem cells (ADSCs) have been widely used in Korea over the last few years by plastic surgeons as a semi-permanent volume expander. In June 2009, the Korean Food and Drug Administration (KFDA) allowed ADSCs to be used as autologous cell transplant when obtained and processed within a medical clinic with minimal processing [1].
Mesenchymal stem cells (MSCs) are found in numerous human tissues including bone marrow, synovial tissue and adipose tissue. These have been shown to differentiate into bones, cartilage, muscle and adipose tissue, representing a promising new area of therapy in regenerative medicine [2].
Because of their potent capabilities, MSCs have been used successfully in animal models to regenerate cartilage and bones [3,4]. In 2008, Centeno and colleagues reported regeneration of knee cartilage in a human by using autologous culture-expanded bone-marrow-derived stem cells [5]. However, to the best of our knowledge ADSCs have never been used successfully in osteonecrosis of a femoral head and in osteoarthritis of a human knee.
Osteonecrosis, or avascular necrosis, of femoral head is relatively a common disorder affecting individuals in their 30s to 50s. Osteoarthritis of a knee is an even more common disorder, especially in older patients. Currently, the only cure for both diseases is surgical intervention. However, the successful regeneration of bones and cartilage with ADSCs may represent a promising new, minimally invasive, non-surgical alternative.
Many issues need to be resolved and clarified before the general application of the procedure. The mechanism of regeneration is not yet clear. It could be through direct differentiation of stem cells that were introduced to the diseased joints. Alternatively, it could be due to the tropic effects of ADSCs on the existing tissues. Further, various elements of the local environment can affect the differentiation of MSCs [6]. Also, it is believed that a scaffolding material might be needed to allow the MSCs to attach and engraft [7].
Platelet-rich plasma (PRP) was used as a growth factor and as a differentiating agent for the MSCs. PRP contains multiple growth factors including transforming growth factor(TGF)β, insulin-like growth factor (IGF), fibroblast growth factor (FGF), and platelet-derived growth factor (PDGF). A literature review of the data on PRP shows that it has a positive effect on the stimulation of Bones, Blood vessel and Chondrocyte formation [8-10]. Hyaluronic acid was added as a Scaffolding material, and Calcium chloride was used as a PRP-activating agent [11].
This series of case reports demonstrates successful clinical results of regenerating bones in osteonecrosis and cartilage in patients with osteoarthritis, using percutaneously implanted, autologous MSCs along with PRP, hyaluronic acid, calcium chloride (CaCl2) and very-low-dose dexamethasone.
Case presentations
The following cases concern four different individuals. Of the four, the first two cases involve bone regeneration in osteonecrosis of hips, the latter two cases regeneration of cartilage in osteoarthritis of knees.
The first case concerns a 29-year-old Korean woman with over a year's history of right hip pain due to osteonecrosis.
Approximately a year prior to presentation, she started having hip pain with no history of trauma. She was seen by a physician and was diagnosed with osteoarthritis of the hip after an MRI scan. After taking non-steroidal anti-inflammatory drugs (NSAIDs) for a few weeks, her hip pain improved. About a month prior to presentation, she again started having hip pain radiating to the anterior region of the right knee. The pain was worse when standing up, walking, and exercising. The pain improved with rest. However, this time, the pain was not greatly relieved with NSAIDs.
A repeat MRI showed osteonecrosis of the femoral head, stage 4. Since there is no effective non-surgical treatment of the disease, she elected to receive stem cell treatment.
At the time of initial evaluation, she reported moderately severe pain (visual analog scale (VAS) score 7) on rest, increased pain when standing and walking (VAS score 9).
For a week prior to liposuction, she was Restricted from taking corticosteroids, aspirin, NSAIDs, and oriental herb medications.
For the liposuction procedure, she was brought into an operating room and placed in a supine position. She was then sedated with Propofol 2 mg intravenously (push) and a 20 mg/hour rate of continuous infusion.
After cleaning her abdominal area with povodine-iodine and placing sterile drapes, an incision of approximately 0.5 cm was made approximately 5 cm below the umbilicus. Then, using Tumescent solution (500 cm3 Normal saline, 40 cm3 2% Lidocaine, 20 cm3 0.5% Marcaine, 0.5 cm3 Epinephrine 1:1000), the Lower abdomen area was anesthetized. Next, using a 3.0 Hartman cannula, a total of 160 cm3 of lipoaspirates were extracted and separated by gravity. The resulting 100 cm3 of adipose tissue was then Centrifuged at 3500 rpm for Five minutes. The end result was approximately 40 cm3 of packed adipose tissue, fibrous tissue, red blood cells and a small number of nucleated cells.
An equal volume of digestive enzyme, 0.07% collagenase type 1, composed of several collagenases, sulfhydryl protease, clostripain, a trypsin-like enzyme, and an amino peptidase, derived from Clostridium histolyticum (Adilase; Worthington, Lakewood, NJ, USA) was then mixed with the centrifuged lipoaspirates at a ratio of 1:1 and Digested for 30 minutes at 37°C while rotating [12].
Bacterial collagenases differ from vertebrate collagenases in that they exhibit broader substrate specificity [13].
After the digestion, the lipoaspirates were Centrifuged at 100g for three minutes to separate the lipoaspirate and the enzyme. The leftover enzyme was then removed.
Using 500 cm3 5% dextrose in lactated Ringer's solution, the lipoaspirates were washed three times to remove the collagenase. After each washing, the lipoaspirates were centrifuged at 100 g. After the last centrifuge process, approximately 10 cm3 of ADSCs were obtained.
While preparing the ADSCs, 30 cm3 of autologous blood was drawn with 2.5 cm3 of anticoagulant citrate dextrose solution (ACD) formula. This was Centrifuged at 200 g for Five minutes. The resultant supernatant was drawn and Centrifuged at 1000 g for Five minutes. The supernatant was drawn and discarded. The resulting buffy coat was mixed with 10 cm3 of ADSCs.
Hyaluronic acid 1 cm3 was added to this mixture to act as a scaffold. This PRP was again mixed with CaCl2 for activation of platelets at a ratio of 10:2 (PRP 10:2 CaCl2).
In order to inject the mixture of stem cells and PRP, our patient was first placed in a lateral position with her left side down. After cleaning with povodine-iodine and draping with sterile drapes, 2% Lidocaine was used to anesthetize the hip at the femoral head region. Using a 22-gauge 3.5-inch needle, 17 cm3 mixture of ADSCs, PRP, Hyaluronic acid and CaCl2 were injected into the femoral head under ultrasound guidance.
She was then instructed to remain still with her leg elevated for 30 minutes to allow for cell attachment. On discharge home, she was instructed to maintain activity as tolerated. She returned to the clinic for four additional PRP injections with Calcium chloride every week over a period of a month.
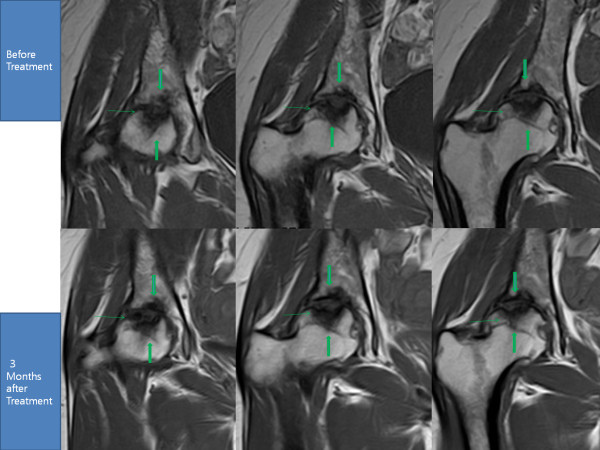
After the fourth week of the ADSC injection, her pain had improved more than 50%. By week 12, her pain had improved more than 70% along with an improvement in range of motion (Tables 1 and 2). A repeat MRI taken at week 12 showed a significant filling of bone defects on the superior acetabulum and probable bone matrix formation in the subcortical region of the femoral head (Figure 1).
Table 1. Functional rating index [16] and visual analog scale (VAS) score for patient 1
Table 2. Physical therapy (PT) range of motion of patient 1
Figure 1. MRI of the right hip; T1 sequential coronal views. The cavity surrounded by the three green arrows has decreased in size in post-treatment MRIs due to probable bone regeneration.



 留言列表
留言列表
